Key findings
- Young adults are nearly twice as likely to be impacted by policies that take coverage away from people who don’t meet a work requirement as all Medicaid enrollees; over 40,000 young Kentuckians could lose coverage
- Policies that take coverage away from people who don’t meet a work requirement disproportionately impact young African Americans
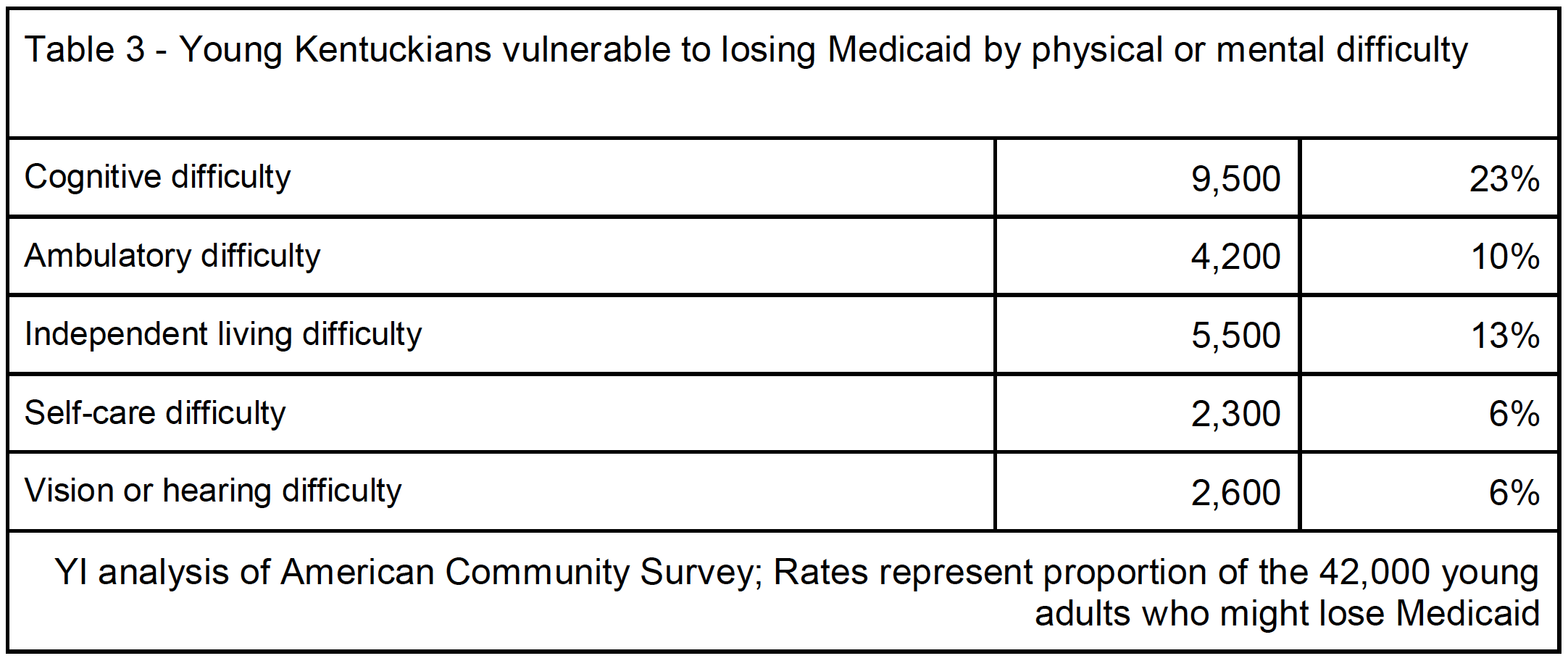
- Many of those vulnerable to losing coverage suffer from physical difficulties, including nearly a quarter with cognitive difficulty
- Many who could lose coverage do work, including those working blue-collar jobs and in childcare
Introduction
All across the country, states are moving to adopt policies that take coverage away from people who don’t meet a work requirement. Proponents of this policy cite stewardship of taxpayer dollars as one justification, which is odd because, in the big picture, work requirements won’t actually save that much money. The majority of Medicaid enrollees are either kids, elderly, disabled, or already working, so the target population is relatively small compared to the size of the program overall. For instance, Virginia estimated that implanting a work requirement could cost as much as $23.1 million per year. Studies suggest work requirements don’t even increase employment in the long -run.
But whatever their motivation, many states are pushing work requirements for Medicaid, and the stakes are high for those individuals in the crosshairs: Nationally, up to 4 million people could lose coverage if all states implemented work requirements. With a growing number of states proposing work requirements for Medicaid we wanted to take a closer look at the young adults there who could lose coverage. (You can also read YI’s official comments of the impact on young adults here).
This blog takes a close look at Kentucky’s proposed rule and profiles the young people that might get thrown off the program because they don’t work enough hours to meet the proposed requirement (even those who meet the requirements could lose coverage, too, but we focus on the ones who currently don’t meet the requirement). We wanted to highlight some of the details about this population, so that policymakers in Kentucky and elsewhere had a better idea of the impact of their policies. In fact, in his decision to block Kentucky’s policy, a federal judge concluded that policymakers “never adequately considered” the impact of the work requirements “to help the state furnish medical assistance to its citizens, a central objective of Medicaid.”
Impact
Using U.S. Census data, we estimate that of the 1.2 million Medicaid beneficiaries in Kentucky, around 245,000, or about 20 percent, are between the ages of 19 and 34 years old. According to the policy proposed in Kentucky, a little over 150,000 young Medicaid participants would be exempt from work requirements because they’re either in school, taking care of children, or receiving social security income or dually enrolled in Medicare. That leaves 95,000 young adults who could lose their coverage in Kentucky, though some could qualify for other exemptions not modelled here related to pregnancy, medical frailty, substance use disorder, or other qualifying conditions. That’s 39 percent of the young Medicaid population that could lose coverage. Only 21 percent of the Medicaid population overall would be subject to the work requirement, making young adults nearly twice as likely as other Medicaid enrollees to be impacted. Even those who work enough hours could lose their coverage, due to the burden of reporting and verifying their time.
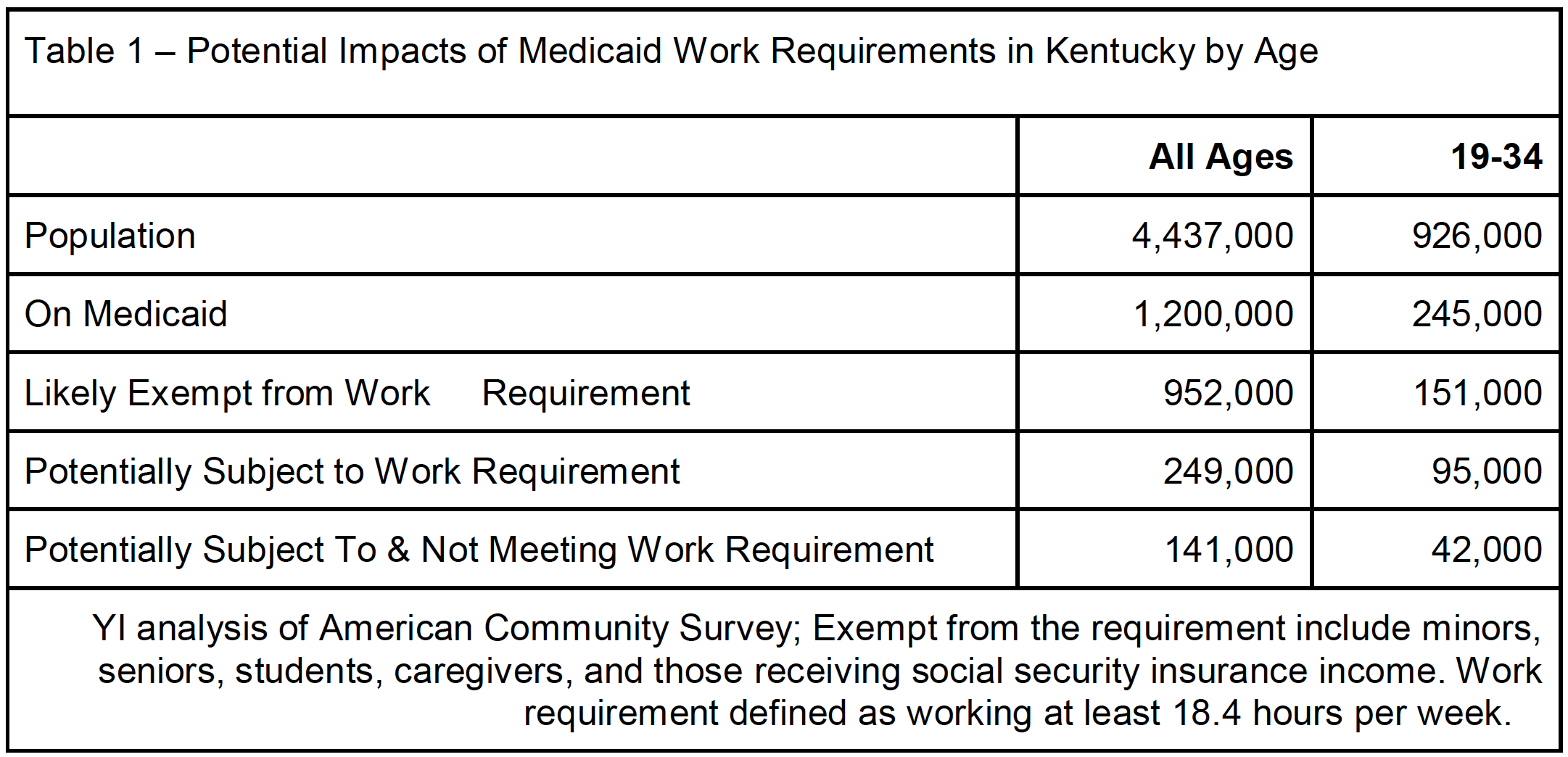
Of those 95,000 young adults who would potentially have to work to stay on Medicaid, we estimate that nearly 42,000 would not meet the new requirements. This has serious implications, as coverage comes with preventive care that can help young people avoid chronic health problems down the road. This also demonstrates how important it is for young people to get involved and have their voices heard in this policy debate.
Profile of young adults who would not meet work requirements
When looking at sterile tables of data, it can be easy to forget that we’re talking about real people with individual experiences and challenges. Census data can’t tell us everything about people’s’ lives, but can sketch an outline of who it is we’re talking about. We hope these details about the 42,000 young adults who would lose their coverage paint a clearer picture of the impacts of work requirements:
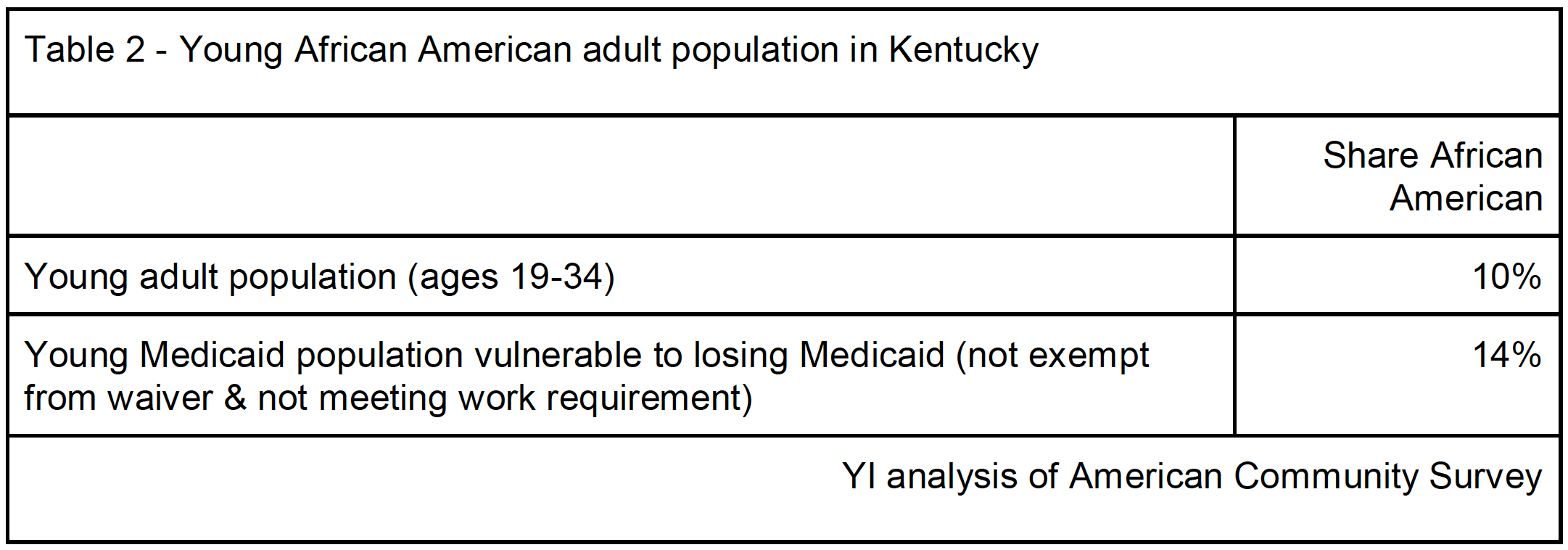
Black Kentuckians: Young African Americans make up 10 percent of the young adult population in Kentucky, but 14 percent of young adults who could lose coverage are African American. Considering black Kentuckians are already uninsured at higher rates than whites (9 percent and 6 percent respectively), adding work requirements to Medicaid stands to exasperate these inequities.
Nearly a quarter suffer from cognitive disability or difficulty: Of the 42,000 young Medicaid enrollees who could lose coverage, nearly 10,000, or almost a quarter, report difficulty remembering, learning, concentrating, or making decisions because of a physical, mental, or emotional condition. Another 5,000 have difficulty performing basic physical activities, such as walking, climbing stairs, reaching, lifting, or carrying. Another 2,500 are partially or completely blind or deaf. Policymakers should consider the difficulty these individuals might have in finding work and whether taking away their Medicaid is really a policy they want to stand behind.
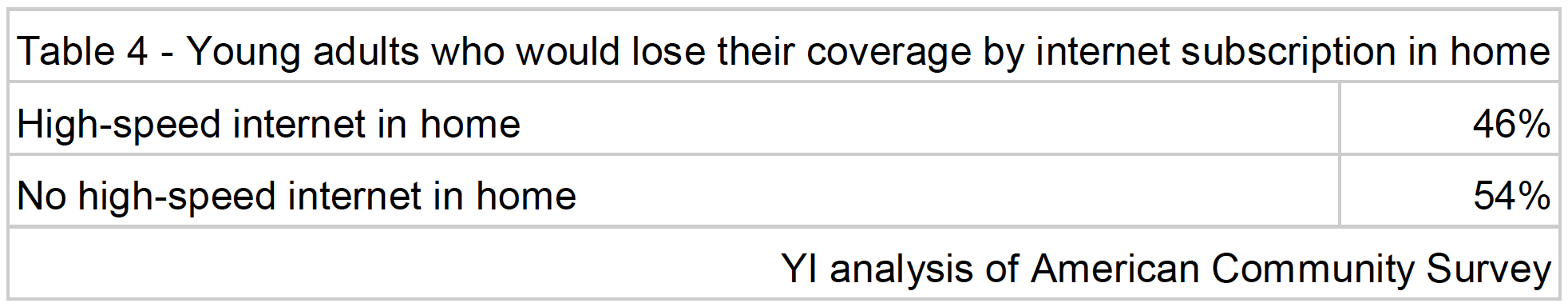
Lack of high-speed internet connection: Despite stereotypes of young adults being constantly connected to technology, over half (20,000) of all those young adults that could lose Medicaid don’t have high-speed internet in their home. A lack of a reliable internet connection hampers one’s ability to find a job and meet the requirement. Also, if enrollees have to verify their hours worked through an online portal, a lack of reliable internet at home will hamper their ability to report hours worked, potentially endangering their benefits even if they do work enough hours.
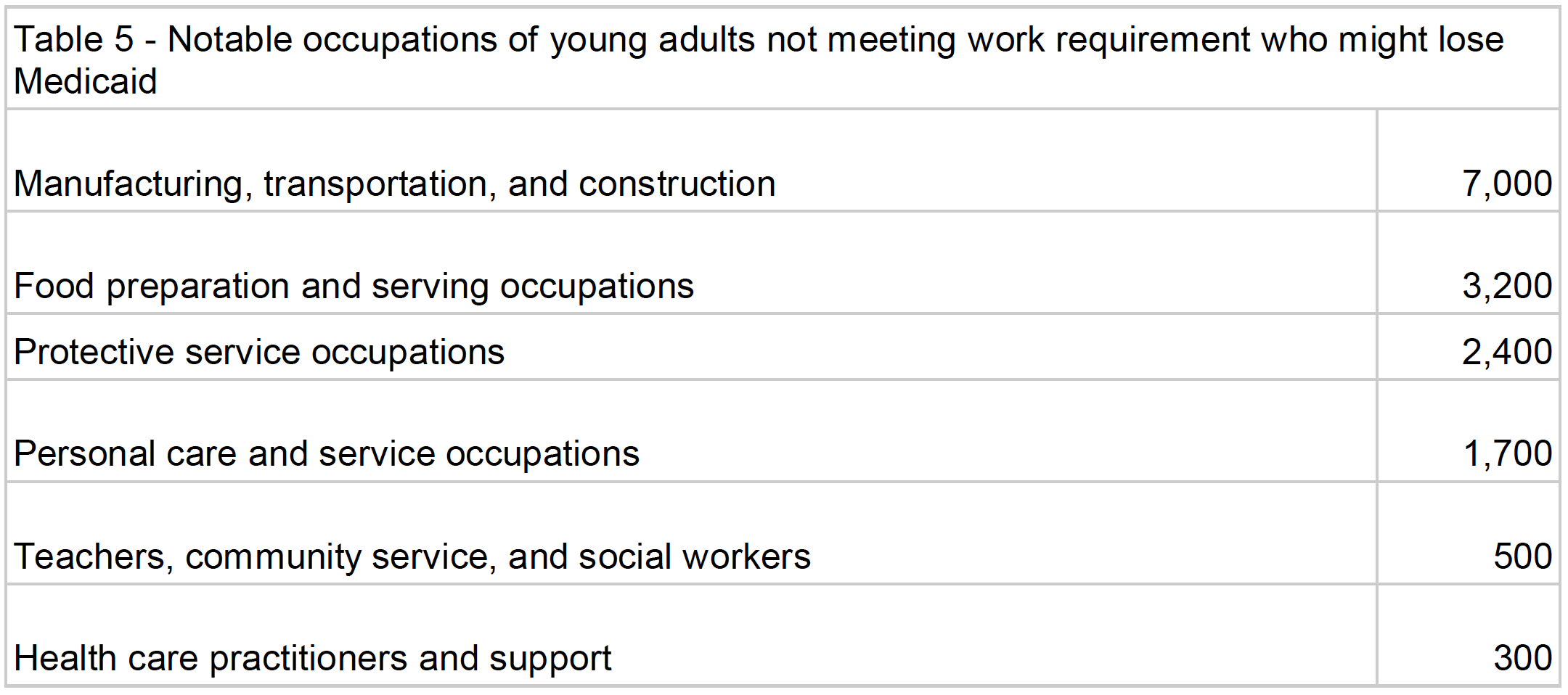
Many already work blue-collar jobs, protect communities, or care for children: About half (22,000) of those young adults who might lose their Medicaid already work, but may not always work the hours necessary to keep their coverage (For more analysis on the work patterns and access to employer-sponsored insurance for the working, non-exempt population, see this brief). Of these workers, about 17 percent work in manufacturing, transportation, and construction. Over 2,000 young people are part-time security officers, firemen, or working other protective service jobs. Over 1,500 young adults work as childcare workers and home health aides. These jobs share a common factor; their hours can be unpredictable and difficult to validate.
Conclusion
Adding work requirements to Medicaid harms many aspects of a state’s economy and society. While our research shows the racial, physical, social, and economic diversity of those vulnerable to losing coverage, they have one thing in common: economic hardship. It’s important to remember that all Medicaid beneficiaries are low-income, earning incomes right around the poverty line. These people don’t have a lot options when it comes to health insurance, and Medicaid coverage can mean the difference between getting the care you need and going without. It could be the difference between life and death.
Before other states consider adopting these sorts of rules, they should ask themselves whether they’d like it if the part-time childcare worker taking care of their child lost their health insurance. Or if they think it’s fair for someone with physical or mental difficulties to lose their coverage because they couldn’t find a job.
Methodology
YI used the American Community Survey, a large annual survey fielded by the U.S. Census Bureau. The variables in the American Community Survey do not perfectly reflect the rules of the work requirement in Kentucky, but are the best proxies available in one of the most statistically powerful and publicly available datasets in the country.
To isolate those who might lose coverage, our model starts with identifying the entire Medicaid population in Kentucky. We then assign individuals as exempt from the work requirement if they meet just one of these criteria:
1) are under 18 years old
2) are over 64 years old
3) are students
4) have children in their household
5) receive social security income
It’s possible that individuals with cognitive, ambulatory, or other difficulties could be exempt from the requirement due to the “medically frail” exemption, but Kentucky has not defined that designation, therefore we designate those individuals as non-exempt. Also, the parent exemption limits one caregiver per household, so our analysis over-counts the number of individuals exempt from the work requirement.
The Kentucky rule requires enrollees to work 80 hours per month. The ACS captures how many hours individuals usually worked per week. So we set the threshold for meeting the work requirement at 18.4 hours per week.
